Overview
A pacemaker is a small electronic device implanted in the chest to help regulate abnormal heart rhythms. This life-saving device is often recommended for those experiencing bradycardia (slow heart rate), arrhythmias, or heart failure symptoms. At Revive Heart Institute, we specialize in pacemaker implantation in Mumbai for patients with heart rhythm disorders requiring timely intervention.
A pacemaker is also called a Cardiac Pacing Device.
Types
Depending on your condition, you might have one of the following types of pacemakers.
Single chamber pacemaker. This type usually carries electrical impulses to the right ventricle of your heart.
Dual chamber pacemaker. This type carries electrical impulses to the right ventricle and the right atrium of your heart to help control the timing of contractions between the two chambers.
Biventricular pacemaker. Biventricular pacing, also called cardiac resynchronization therapy, is for people who have heart failure and heartbeat problems. This type of pacemaker stimulates both of the lower heart chambers (the right and left ventricles) to make the heart beat more efficiently.
Why it's done?
A pacemaker is implanted to help control your heartbeat. Your doctor may recommend a temporary pacemaker when you have a slow heartbeat (bradycardia) after a heart attack, surgery or medication overdose but your heartbeat is otherwise expected to recover. A pacemaker may be implanted permanently to correct a chronic slow or irregular heartbeat or to help treat heart failure.
How your heart beats?
The heart is a muscular, fist-sized pump with four chambers, two on the left side and two on the right. The upper chambers (right and left atria) and the lower chambers (right and left ventricles) work with your heart's electrical system to keep your heart beating at an appropriate rate — usually 60 to 100 beats a minute for adults at rest.
Your heart's electrical system controls your heartbeat, beginning in a group of cells at the top of the heart (sinus node) and spreading to the bottom, causing it to contract and pump blood. Aging, heart muscle damage from a heart attack, some medications and certain genetic conditions can cause an irregular heart rhythm.
What a pacemaker does?
Pacemakers work only when needed. If your heartbeat is too slow (bradycardia), the pacemaker sends electrical signals to your heart to correct the beat.
Some newer pacemakers also have sensors that detect body motion or breathing rate and signal the devices to increase heart rate during exercise, as needed.
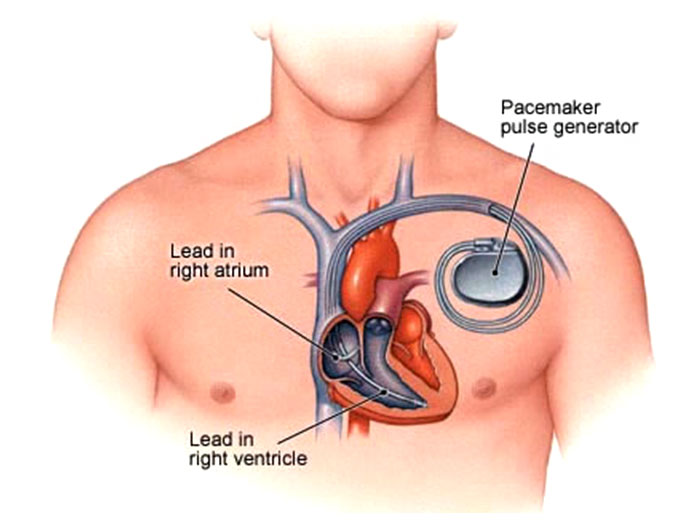
A pacemaker has two parts:
Pulse generator. This small metal container houses a battery and the electrical circuitry that controls the rate of electrical pulses sent to the heart.
Leads (electrodes). One to three flexible, insulated wires are each placed in one or more chambers of the heart and deliver the electrical pulses to adjust the heart rate. However, some newer pacemakers don't require leads. These devices, called leadless pacemakers, are implanted directly into the heart muscle.
How you prepare?
Before your doctor decides if you need a pacemaker, you'll have several tests done to find the cause of your irregular heartbeat. Tests done before you get a pacemaker could include:
Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. Sticky patches (electrodes) are placed on the chest and sometimes the arms and legs. Wires connect the electrodes to a computer, which displays the test results. An ECG can show if the heart is beating too fast, too slow or not at all.
Holter monitoring. A Holter monitor is a small, wearable device that keeps track of the heart's rhythm. Your doctor may want you to wear a Holter monitor for 1 to 2 days. During that time, the device records all of your heartbeats. Holter monitoring is especially useful in diagnosing heartbeat problems that occur at unpredictable times.
Echocardiogram.This noninvasive test uses sound waves to produce images of the heart's size, structure and motion.
Stress test. Some heart problems occur only during exercise. For a stress test, an electrocardiogram is taken before , during and immediately after walking on a treadmill or riding a stationary bike.
Sometimes, a stress test is done along with echocardiography or nuclear imaging. It is done to look at the rhythm and ECG changes during physical stress.
What you can expect?
You'll likely be awake during the surgery to implant the pacemaker, which typically takes a few hours. A specialist will insert an IV into your forearm or hand and give you a medication called a sedative to help you relax. Your chest is cleaned with special soap.
Most pacemaker implantations are done using local anesthesia to numb the area of the incisions. However, the amount of sedation needed for the procedure depends on your specific health conditions. You may be fully awake or lightly sedated, or you may be given general anesthesia (fully asleep).
One or more wires are inserted into a major vein under or near your collarbone and guided to your heart using X-ray images. One end of each wire is secured at the appropriate position in your heart, while the other end is attached to the pulse generator, which is usually implanted under the skin beneath your collarbone.
A leadless pacemaker is smaller and typically requires a less invasive surgery to implant the device. The pulse generator and other pacemaker parts are contained in a single capsule. The doctor inserts a flexible sheath (catheter) in a vein in the groin and then guides the single component pacemaker through the catheter to the proper position in the heart.
You'll likely stay in the hospital for a day after having a pacemaker implanted. Your pacemaker will be programmed to fit your heart rhythm needs. You'll need to arrange to have someone drive you home from the hospital.
Your doctor might recommend that you avoid vigorous exercise or heavy lifting for about a month. Avoid putting pressure on the area where the pacemaker was implanted. If you have pain in that area, ask your doctor about taking .
Results
Having a pacemaker should improve symptoms caused by a slow heartbeat such as fatigue, lightheadedness and fainting. Because most of today's pacemakers automatically adjust the heart rate to match the level of physical activity, they may can allow you to resume a more active lifestyle.
Your doctor should check your pacemaker every 3 to 6 months. Tell your doctor if you gain weight, if your legs or ankles get puffy, or if you faint or get dizzy.
Your pacemaker's battery should last 5 to 15 years. When the battery stops working, you'll need surgery to replace it. The procedure to change your pacemaker's battery is often quicker and requires less recovery time than the procedure to implant your pacemaker.
What is ICD ?
ICD stands for implantable cardioverter-defibrillator. Sometimes your heart might go into very fast /irregular heart beat. ICD is the device similar to pacemaker. It has additional property of given small shock to the heart if the heart beats go very high or irregular ( arrhythmias ).
How long does the battery of pacemaker / ICD last?
The life of battery of pacemaker depends on the frequency and voltage of usage.
Pacemaker and death and cremation?
The pacemakers and ICD harbor a small battery. These batteries are known to explode during cremation. Hence , it is important to inform the doctor upon death of the patient . The care taker of the crematorium should also be informed about the pacemaker.
Choose the Best Pacemaker Surgeon in Mumbai
At Revive Heart Institute, our team is led by some of the best pacemaker surgeons in Mumbai, offering expert care, advanced technology, and personalized follow-up for every patient. Whether you need a single chamber pacemaker, a CRT device, or require permanent pacemaker implantation in Mumbai, we ensure a smooth and safe treatment journey.
