
A heart transplant, or a cardiac transplant in Mumbai, is a surgical transplant procedure performed on patients with end-stage heart disease or .
A heart transplant in Mumbai is an operation in which a failing heart is replaced with a healthier donor heart. The most common procedure is to take a functioning heart, with or without both lungs, from a recently deceased organ donor (brain death is the standard) and implant it into the patient. The patient's own heart is either removed and replaced with the donor heart (orthotopic procedure) or, much less commonly, the recipient's diseased heart is left in place to support the donor heart (heterotopic, or "piggyback", transplant procedure).
Heart transplant is a life-saving treatment intended to improve the quality and duration of life for a recipient.
While a heart transplant is a major operation, your chance of survival is good with appropriate follow-up care.
Why it's done
Heart transplants are performed when the heart failure doesn’t respond to the medical line of treatment.
Another organ transplant may be performed at the same time as a heart transplant (multiorgan transplant) in people with certain conditions at select medical centers.
Multiorgan transplants include:
Heart-kidney transplant. This procedure may be an option for some people with kidney failure in addition to heart failure.
Heart-liver transplant. This procedure may be an option for people with certain liver and heart conditions.
Heart-lung transplant. Rarely, doctors may suggest this procedure for some people with severe lung and heart diseases if the conditions cannot be treated with only a heart transplant or a lung transplant.
Can I get a heart transplant?
A heart transplant is not right for everyone. Your doctor would run some test to check your bloods and other investigations to see if you could get heart transplant. Doctor might perform test to check pressures in your lungs ( right heart catheter ). You might not be a good candidate for a heart transplant if you:
- Are at an advanced age that would interfere with the ability to recover from transplant surgery
- Have another medical condition that could shorten your life, regardless of receiving a donor heart, such as a serious kidney, liver or lung disease
- Have an active infection
- Have a recent personal medical history of cancer
- Are unwilling or unable to make lifestyle changes necessary to keep your donor heart healthy, such as not using recreational drugs, not smoking and limiting alcohol use
What if I am not a candidate for heart transplant?
For some people who cannot have a heart transplant, another option may be a ventricular assist device (VAD) or commonly called as left ventricular assists devices ( LVAD ).
A VAD is a mechanical pump implanted in your chest that helps pump blood from the chambers of your heart (ventricles) to the rest of your body.
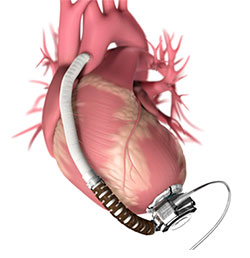
VADs are commonly used as temporary treatments for people waiting for heart transplants. These devices are increasingly being used as long-term treatment for people who have heart failure but are not eligible for heart transplants. If a VAD doesn't help your heart, doctors may sometimes consider a total artificial heart — a device that replaces the ventricles of your heart — as an alternative short-term treatment while you're waiting for a heart transplant.
What happens during heart transplant surgery?
Heart transplant surgery is an open-heart procedure that takes several hours. If you've had previous heart surgeries, the surgery is more complicated and will take longer.
You'll receive medication that causes you to sleep (general anesthetic) before the procedure. Your surgeon will make an incision in your chest. Your surgeons will connect you to a heart-lung bypass machine to keep oxygen-rich blood flowing throughout your body.
Your surgeon then removes the diseased heart and sews the donor heart into place. He or she then attaches the major blood vessels to the donor heart. The new heart often starts beating when blood flow is restored. Sometimes an electric shock is needed to make the donor heart beat properly.
You'll be given medication to help with pain control after the surgery. You'll also have a ventilator to help you breathe and tubes in your chest to drain fluids from around your lungs and heart. After surgery, you'll also receive fluids and medications through intravenous (IV) tubes.
You'll initially stay in the intensive care unit (ICU) for a few days, then be moved to a regular hospital room. You're likely to remain in the hospital for 2 weeks or more. The amount of time spent in the ICU and in the hospital varies from person to person.
After you leave the hospital, your transplant team will monitor you. Due to the frequency and intensity of the monitoring, many people stay close to the transplant center for the first three months. Afterward, the follow-up visits are less frequent, and travel is easier.
What happens after heart transplant?
You'll be monitored for any signs or symptoms of rejection, such as shortness of breath, fever, fatigue, not urinating as much or weight gain. It's important to let your transplant team know if you notice any signs or symptoms of rejection or infection.
To determine whether your body is rejecting the new heart, you'll have frequent heart biopsies in the first few months after heart transplantation, when rejection is most likely to occur. The frequency of necessary biopsies decreases over time.
During a heart biopsy, a doctor inserts a tube into a vein in your neck or groin and directs it to your heart. The doctor runs a biopsy device through the tube to remove a tiny sample of heart tissue, which is examined in a lab.
You'll need to make several long-term adjustments after you have had your heart transplant. These include:
Taking immunosuppressants. These medications decrease the activity of your immune system to prevent it from attacking your donated heart. You'll take some of these medications for the rest of your life.
Because immunosuppressants render your body more vulnerable to infection, your doctor might also prescribe antibacterial, antiviral and antifungal medications. Some drugs could worsen — or raise your risk of developing — conditions such as high blood pressure, high cholesterol, cancer or diabetes.
Over time, as the risk of rejection decreases, the doses and number of anti-rejection drugs can be reduced.
Managing medications and a lifelong care plan. After a heart transplant, taking all your medications as your doctor instructs and following a lifelong care plan are vital.
A daily routine for taking your medications may be helpful. Keep a list of all your medications with you at all times for medical appointments and in case you need emergency care. Check with your doctor before you use any nonprescription medicines, vitamins, supplements or herbal products.
Your doctor might give you instructions regarding your lifestyle. Recommendations may include wearing sunscreen, exercising, eating a healthy diet and being careful to lower your risk of infection. You doctor may also recommend that you not use tobacco products or recreational drugs and limit alcohol use.
Follow all of your doctor's instructions, see your doctor regularly for follow-up appointments, and let your doctor know if you have signs or symptoms of complications.
Cardiac rehabilitation. This program incorporates exercise and education to help you improve your health and recover after a heart transplant. Cardiac rehabilitation can help you regain your strength and improve your quality of life. You may start it before you leave the hospital.
How are the results of heart transplant?
Most people who receive a heart transplant enjoy a good quality of life. Depending on your condition, you may be able to resume many of your daily life activities, such as work, hobbies and sports, and exercising. Discuss with your doctor what activities are appropriate for you.
Some women who have had heart transplants could become pregnant. However, talk to your doctor if you're thinking about having children after your transplant. You'll likely need medication adjustments before becoming pregnant, as some medications can cause pregnancy complications.
Survival rates after heart transplantation vary based on a number of factors. Survival rates continue to improve despite an increase in older and higher risk heart transplant recipients. Worldwide, the overall survival rate is about 90% after one year and about 80% after five years for adults.
What if your new heart fails?
Heart transplants aren't successful for everyone. Your new heart can fail for a number of reasons. Your doctor might then suggest adjusting your medications or, in more extreme cases, having another heart transplant.
If additional treatment options are limited, you might choose to stop treatment. Discussions with your heart transplant team, doctor and family should address your expectations and preferences for treatment, emergency care and end-of-life care.
What could go wrong?
Some patients might experience complications or problems either during the operation or in the days or weeks following a heart transplant
- Rejection:
Rejection is when your body’s immune system starts to ‘attack’ your new heart. The body thinks that the new heart is a foreign thing which should not be in the body hence tries to act against it. Even if you take your anti-rejection medications carefully, rejection can still occur. - The new Heart not pumping well
This could happen in few of patients undergoing heart transplant. There could be multiple reasons for it. If this happens , you would be put on a external heart lung machine called as an ECMO to support the heart till it recovers. - Uncontrolled diabetes:
If you have diabetes before the heart transplant, it is likely that your blood sugar will be more difficult to control after the transplant. - Stroke:
A stroke (a blockage of the blood supply to the brain) can happen soon after a transplant. Strokes are more common in older patients, and in those who have had a stroke before. Like wise there are chances you have clots in your veins. - You might not survive heart transplant
Important Links: Best Heart Surgeon in Prabhadevi | Best Bypass Surgeon In Prabhadevi | Best Cardiologist In Prabhadevi | Best Tavi in Prabhadevi | Best Angioplasty in Prabhadevi | Best Transplant Doctor in Prabhadevi
